If you suffer from recurring back pain and your focus on strengthening your core doesn’t seem to work then perhaps it is time to take a different approach to prevent your lower back pain from recurring.
For at least the last 20 years there has been a focus on advising people to strengthen their core stability muscles that in turn will prevent back pain. However the research to support this is thin at best. Much of the research has been carried out on small non representative samples (1). When the samples are representative then whilst some short term benefits can be found no long term benefits (over 6 months) can be seen (2) in back pain prevention. Alternatively it was found that core stability rehab is no more effective than general exercise (3).
Does the following scenario sound familiar?
I hear this quite frequently from my patients.
A patient has experienced back pain and through their physical therapist they have been given a series of cores stability exercises. Such as ‘The bridge’, the ‘1 legged bridge’, ‘the plank’, ‘superman’ etc. The patient has done them frequently and noted increased muscle tone and an ability to do the exercises for longer or more frequently. However 6-12 months later they have a recurrence of their back pain.The patients blame themselves for not doing the exercises correctly or not frequently enough. Wait for the pain to subside, perhaps receive some treatment then carry on with the same exercises.
If you can relate to this then may be it’s time to take a different approach. After all Einstein’s definition of insanity is doing the same thing over again and expecting a different outcome!
What’s the thinking behind Core stability exercises?
In essence the theory is by activating your core stability muscles such transverse obliques, rectus abdominus, pelvic floor, internal and external obliques, diaphragm you can help support the lumbar spine and so help reduce its work load. However if the research is right and there is a lack of effectiveness then perhaps we need to ask the question ‘Why can’t our backs cope with the work load in the first place?’And – “Why does it need extra support?”
An Alternative approach
I would argue that the area of your spine that is in pain is a result of it trying to cope with extra work load because other parts of the spine or body are not moving as well as they should.
The body has this amazing ability to adapt and deal with reduced function in one part of the body to maintain our overall function. The spine is a key part of this.
 24 interlinking segments that act liked a coiled spring. If a section of the coil stops moving then the sections above and below move more to ensure our bodies can achieve the movement we require. It’s this extra movement of muscles and joints that over time can lead to muscle fatigue and joint inflammation. These are two main symptoms of lower mechanical back pain.
24 interlinking segments that act liked a coiled spring. If a section of the coil stops moving then the sections above and below move more to ensure our bodies can achieve the movement we require. It’s this extra movement of muscles and joints that over time can lead to muscle fatigue and joint inflammation. These are two main symptoms of lower mechanical back pain.
Address the causes through treatment and rehab
Of all the hundreds of patients that I have seen through my practice with lower back pain the common factors are reduced mobility in the upper back and shoulders and reduced mobility in the pelvis and hips.
Coincidentally these are the two main areas of our body that we keep static for long periods of time every day of the week!
Our sedentary lifestyles reduce our mobility
It is this lack of movement in these two areas that can cause us lower back pain pain in the long term.

upper back stiffness can contribute to lower back pain
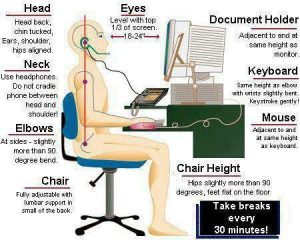
We sit at our desk, shoulders forward, fingers ready to type on our key boards, heads forward, upper back arched. Our hips flexed. Sometimes for hours at a time.
Our bodies take these inputs as a desired position and start to adapt accordingly. The body is always looking for efficiencies to reduce energy expenditure. So it reduces blood supply to muscles. Joints stop moving so nerves receive less innervation.
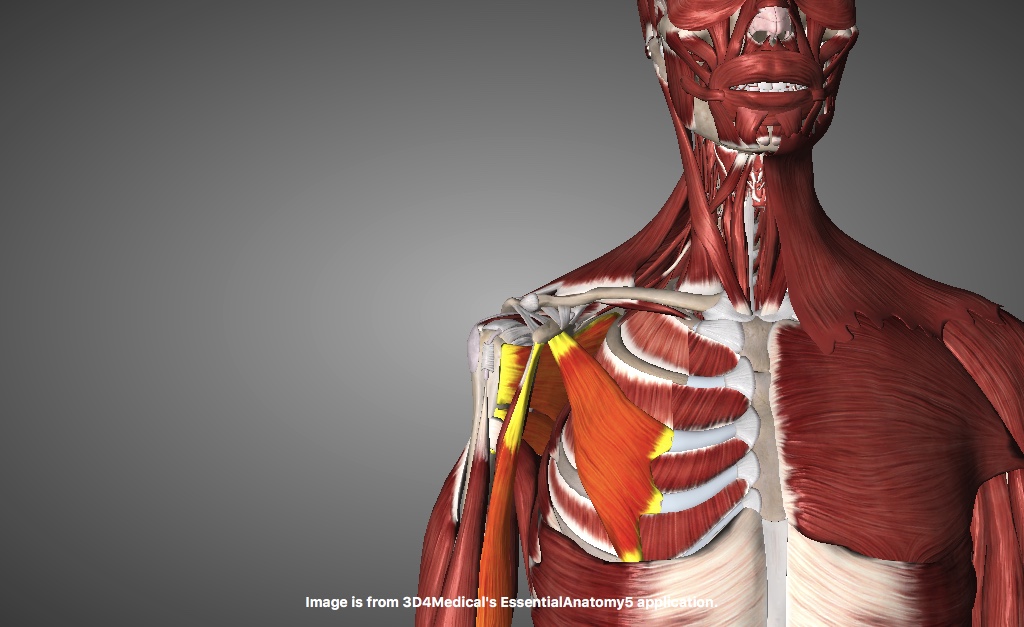
Muscles in our upper backs become fibrotic and joints become less mobile.
We do this day in day out for up to 8 hrs a day for months and even years! Then we go home and watch TV or use our laptops at home, or alternatively try and get the stress of our work out the system and go cycling and assume the exact same position. Or we go to the gym and contract the same muscles that were contracted at our desks (our pectorals and biceps and hip flexors)
Implications for our Lower back
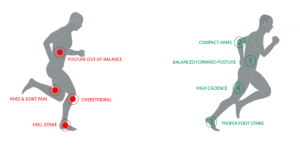
If the middle section of our spine can no longer rotate or bend forward as much as it used to do then the lower back (the lumbar spine) will have to move more to ensure that there is no reduction in functional ability and range of movement.
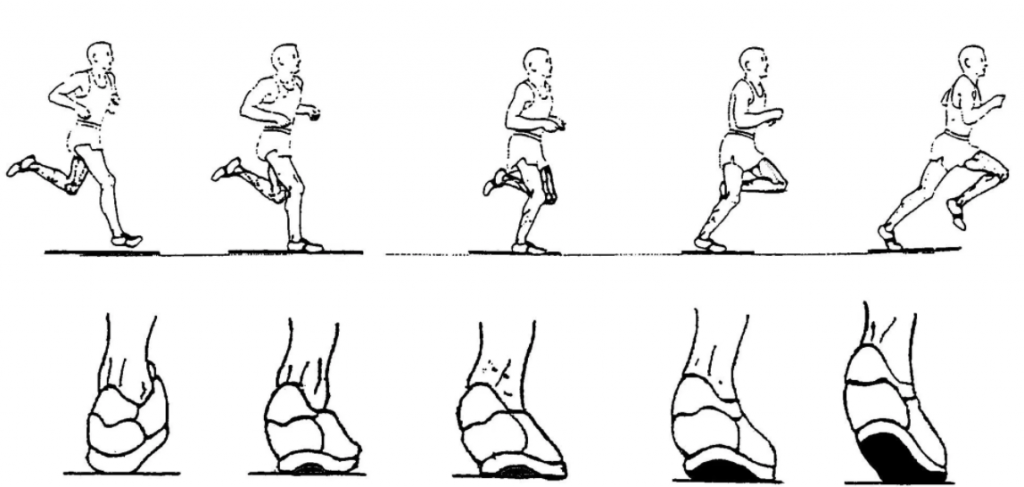
Likewise if we cannot rotate from the hip or our hips are flexed forwards because our hip flexors are permanently contracted from all the sitting down we do then our lower back muscles become more involved in simple daily activities such as walking and standing.
Our bodies make these adaptations without us being aware of them. Day in day out for months and years.
Then add in the role that the lower back was designed for and the wear and tear that can take place without this extra work load and you can start to see why an upper back or hip that can’t move optimally can help increase the risk of fatigue, strain and ultimately, injury in the lower spine.
How can you help?
# Change the inputs in your upper back
From a static 8 hrs. Stop every 30-45 mins and make your upper back and shoulders move. Your body will respond by increasing blood supply. Muscles will change to become more flexible. Joints and innervation inputs will increase.
Here is a simple exercise you can do at work whilst sitting down to start changing the inputs. Do it every 45-60 minutes that you are at your desk. Your colleagues might think you are mad at first but soon they will all start doing it! It really works.
# Change the inputs to our hips and pelvis
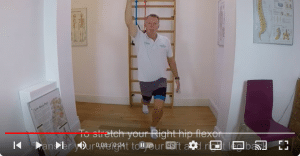
We need to reduce the tightness in our hip flexors that builds up over time as we sit at our desk, cars, TV, dinner table and on our bikes . Here is a really effective exercise to do just that.
Do it daily am and pm 10-15x. Include it into any activity warm ups and warm downs too. Especially after cycling or running.
Next we need to improve the mobility and rotation of the hip as well as activating the gluteals and hamstrings.
This exercise combines hip flexion stretches with hip rotation. Do it am and pm 10-15x for each exercise. These exercises should all be pain free so if you experience pain after or during then just stop and consult your professional physical therapist. For access to more exercises to improve hip mobility go to Resources
To Conclude
If you have been doing your core stability exercises and you have had no recurrence of lower back pain, then please continue but consider if you are really addressing the cause. With our increasingly sedentary lifestyles we are placing increasing work load on our lower backs due to a lack of mobility above and below in our upper backs and hips. So if you are doing core stability exercises then add hip and upper back mobility exercises into the mix. If you are not doing any exercise then start to work on hip and upper back mobility with the above exercises. The exercises should always be pain free. Click here For more advice on how Hugo treats back pain
References
(1)Stuber KJ1, Bruno P, Sajko S, Hayden JA, Clin J Sport Med. 2014 Nov;24(6):448-56. doi: 10.1097/JSM.0000000000000081.Core stability exercises for low back pain in athletes: a systematic review of the literature.
(2) Xue-Qiang Wang,1 Jie-Jiao Zheng,2,* Zhuo-Wei Yu,2 et al. Public Library of Science. 2012; 7(12): e52082.Published online 2012 Dec 17. doi: 1371/journal.pone.0052082A Meta-Analysis of Core Stability Exercise versus General Exercise for Chronic Low Back Pain
(3)George SZ1, Childs JD, Teyhen DS, Wu SS, Wright AC, Dugan JL, Robinson ME. BMC Med. 2011 Nov 29;9:128. doi: 10.1186/1741-7015-9-128.Brief psychosocial education, not core stabilization, reduced incidence of low back pain: results from the Prevention of Low Back Pain in the Military (POLM) cluster randomized trial.
.



















 24 interlinking segments that act liked a coiled spring. If a section of the coil stops moving then the sections above and below move more to ensure our bodies can achieve the movement we require. It’s this extra movement of muscles and joints that over time can lead to muscle fatigue and joint inflammation. These are two main symptoms of lower mechanical back pain.
24 interlinking segments that act liked a coiled spring. If a section of the coil stops moving then the sections above and below move more to ensure our bodies can achieve the movement we require. It’s this extra movement of muscles and joints that over time can lead to muscle fatigue and joint inflammation. These are two main symptoms of lower mechanical back pain.



