Heel Mobility and related back pain
This article describes how a lack of heel mobility can have a related effect on back pain as well as other common foot and heel problems.
Basic Foot biomechanics
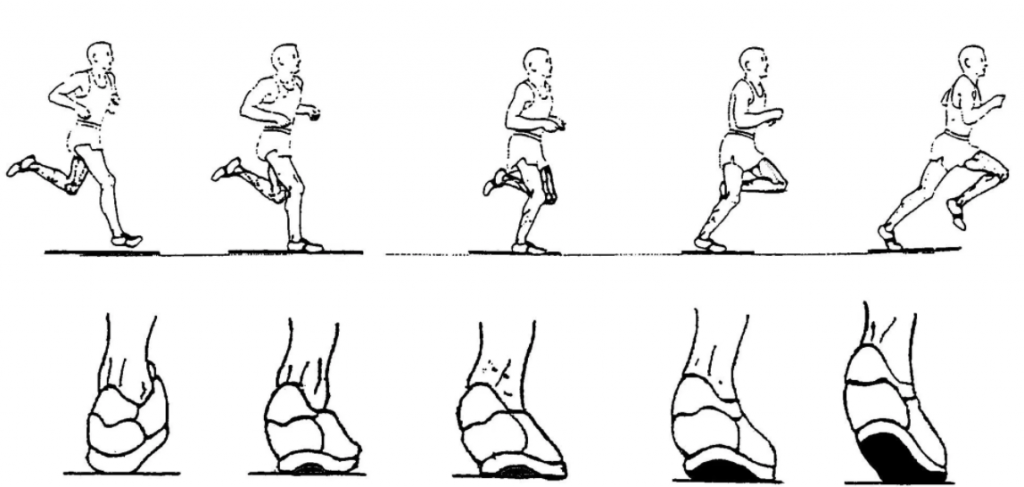
As the heel strikes the ground there should a relatively small inward rotation or ‘pronation’ followed a similar but greater movement of the mid foot (the arch). The force and weight is then transferred to the metatarsals before push off by the big toe and others.

Heel action as we run or walk
Causes of some common foot/heel problems
If the heel does not roll in then the mid foot has to roll further. This in turn increases the stresses through the connective tissue along the base of the foot called the plantar fascia. The lack of movement at the heel also causes greater stress through the Achilles tendon. These increased stresses over time can cause Plantar Fasciitis as well as heel spurs and tendonitis.
This extra roll of the mid-foot has been termed ‘over-pronation’ and it can lead to greater stress and force through the joint at the base of the big toe.
The body responds by laying down more bone in that area to cope with the extra force. The joint becomes larger and the toe is forced inwards forming what is commonly known as a bunion.
How can lack of movement in the heel create back pain and vice versa?
There are two perspectives to consider when looking for causes of heel and back pain.
Ground up forces. That’s to say the forces involved as the heel strikes the ground and the chain reaction of energy and movement as it passes up through the leg to the spine.
Top down forces. That’s to say how gravity acts on our spine and pelvis and how they adapt to cope with it and the effects on the biomechanics of the hip, knee and foot
Top Down
The weight and therefore force of our torso, head and arms is distributed through our lumbar spine and evenly distributed through our pelvis via our sacrum into our legs. To help manage this we have large lumbar vertebrae, thicker discs, strong postural muscles and a matrix of interconnected pelvis and hip muscles such as gluteal muscles and hip flexors and core abdominal muscles.
However with our increasingly sedentary lifestyles our hip flexor muscles can become more contracted and shorter. This can lead to a slight forward tilt in our pelvis.

Fig 1. Forward hip tilt causing internal roll of hips, legs and foot
You can see from Fig 1 how it can increase an inward movement on the upper and lower leg and ultimately encourage increased pronation in the foot. This in turn can lead to foot and lower leg problems described earlier.

Fig 2. Hip tilt due to shortened iliopsoas (hip flexors) and an increased arch (lordosis) of the lower back
Also this can lead to tighter lower back muscles (see Fig 2) and increase the risk of lower back pain.
Ground up
As the heel strikes the ground it is designed to roll inwards. This is called pronation and it is totally natural. The mid foot follows followed by flexion of the toes and especially the big toe.
This inwards roll of the heel bone initiates a subsequent inwards rotation of the lower leg then the upper leg and eventually the hip. It is the inner rotation of the upper femur and hip that gives the gluteal muscle the cue to contract and extend the hip, propelling the body forward to the next step.
Chain reaction
So that first small inwards roll of the heel starts a chain of events culminating in the contraction of the most powerful muscle in the body. However if that inwards roll doesn’t happen then ultimately the gluteal muscle does not contract as efficiently and the lower back postural muscles become involved as they help out the hip to make the next step. That is on top of the job they already have providing stability and mobility to the lumbar vertebrae. A recipe for over work and fatigue of the lower back muscles and ultimately back pain.
Why does the heel become less mobile?
Tight calf muscles can be one cause of restriction of movement into the Achilles tendon which in turn attaches to the heel.

Achilles tendon attaches to heel bone (calcaneus)
A reduced mobility of the calf muscle can be due to a number of reasons. Here are some.
Increased weight: As we get older increase in weight can go onto our tummies. This in turn can change our centre of gravity and bring it slightly forward. Our calf muscles get involved helping to pull us backwards and maintain our balance and CoG over our mid point.
Sports: such as cycling that put a greater load through the calf muscle and in one direction can lead to tight calf muscles
Shoes: that elevate our heels can cause a shortening of our calf muscles. Research has also shown that there is a correlation between high heeled shoes worn and Bunions. The foot is placed in extreme flexion and forces are compressed at the base of the big toes.
A lack of heel movement can also be due to previous ankle injuries: significant ligament strains and fractures can lead to a lack of movement between the joints in our ankles and the heel bone. This in turn can lead to increased load on the calf muscles and tendons.
Implications for effective treatment
In order to effectively treat foot pain and injuries from calf through to big toe Hugo assesses all aspects of the foot, leg, hips and lower back. Evaluation their mobility and ability to move as part of a chain reaction of events.

Sports injury rehab in Kingston and Surbiton
Likewise if back pain is the symptom Hugo will always assess foot and hip movement as part of the process and treat accordingly.
Hugo uses 3D Functional movement exercise as integral part of his treatment to help enhance the movement of joints and muscles and combines this with Osteopathy treatment to improve tissue health and return you back to pain free movement as quickly as possible.


 24 interlinking segments that act liked a coiled spring. If a section of the coil stops moving then the sections above and below move more to ensure our bodies can achieve the movement we require. It’s this extra movement of muscles and joints that over time can lead to muscle fatigue and joint inflammation. These are two main symptoms of lower mechanical back pain.
24 interlinking segments that act liked a coiled spring. If a section of the coil stops moving then the sections above and below move more to ensure our bodies can achieve the movement we require. It’s this extra movement of muscles and joints that over time can lead to muscle fatigue and joint inflammation. These are two main symptoms of lower mechanical back pain.


 k of the leg can increase from occasionally uncomfortable to very painful.
k of the leg can increase from occasionally uncomfortable to very painful.


